telemedicine (telehealth)
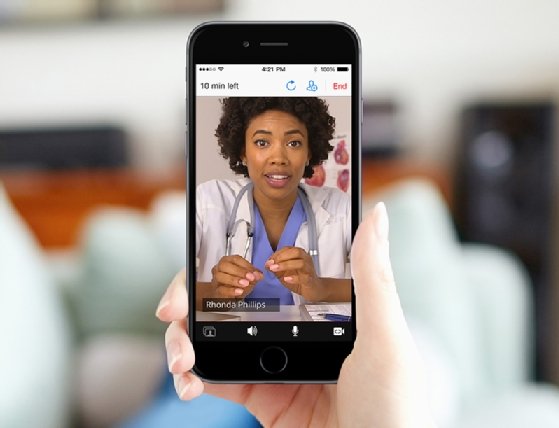
Telemedicine, also referred to as telehealth or e-medicine, is the remote delivery of healthcare services, including exams and consultations, over the telecommunications infrastructure. Telemedicine allows healthcare providers to evaluate, diagnose and treat patients without the need for an in-person visit. Patients can communicate with physicians from their homes by using their own personal technology or by visiting a dedicated telehealth kiosk.
For patients at home, a typical telemedicine exam involves downloading an app such as LiveHealth or calling a telemedicine number, which generally is provided by a primary care physician's office or patient's employer as part of health benefits. After sharing information about medical history and symptoms, the remote patient will be connected to a clinician. Based on the clinician's evaluation, the call will end with the patient receiving further instructions -- such as to take over-the-counter medication, fill a prescription, go to a hospital or schedule a follow-up appointment.
Telemedicine can be classified into three main categories:
- Interactive telemedicine/telehealth - allows physicians and patients to communicate in real time. Such sessions can be conducted in the patient's home or at a designated medical kiosk. Interactions include telephone conversations or the use of video conferencing software that complies with HIPAA regulations.
- Remote patient monitoring - also known as telemonitoring, allows patients to be monitored in their homes using mobile devices that collect data about temperature, blood sugar levels, blood pressure or other vital signs.
- Store-and-forward - also known as asynchronous telemedicine, lets one healthcare provider share patient information, such as lab results, with another healthcare provider.
As various parties seek more efficient ways to provide care at less cost to the patient, telemedicine's role has grown. It is often a time-saving way for a consumer to see and speak to a clinician for minor and non-urgent medical needs instead of going to a primary care physician's office or emergency department. In recent years, many states have passed laws that make telemedicine easier to practice, and federal health regulators are also exploring ways to further grant Medicare reimbursements for telemedicine services.
Advantages of telemedicine
Some of the benefits of telemedicine for patients include:
- Convenience: Patients do not have to take time away from work for an appointment. There is also no travel time or associated expenses, such as paying for gas or child care.
- Increased access: Patients in rural areas can obtain specialty services, such a mental health treatment or post-surgery follow up, that they otherwise might not get without traveling a large distance for an in-person visit. Similarly, patients who live in federally designated, underserved areas have increased access to primary, dental and mental healthcare.
The advantages of telemedicine for providers include:
- Reduced cancellations or no-shows: Because of its convenience for patients, telemedicine can reduce the number of cancellations or no-shows. Providers can reach out prior to or at the appointment time if the patient forgot about the appointment.
- Encourage healthy lifestyle choices: Telemedicine allows providers to encourage their patients' healthy lifestyle choices, such as smoking cessation.
Disadvantages of telemedicine
Some of the challenges of telemedicine include:
- Cybersecurity: As with any technology that involves electronically transmitting patient data, telemedicine systems are susceptible to hackers and breaches. Healthcare organizations remain one of the biggest targets for online criminals and terrorists.
- Inability to prescribe medications: Many states generally do not allow online prescribing (not to be confused with e-prescribing) without an established relationship between the physician and patient. A physical examination or evaluation may be required before a physician can write a prescription for a patient, but there are inconsistencies in state laws as to what constitutes a physical examination.
- Technical training and equipment: Providers need to be trained on how to use telemedicine equipment. There are also the associated costs of the equipment, such as integrated telemedicine carts and encounter management software, to consider. The startup cost of implementing telemedicine may be especially prohibitive to rural facilities.
- Licensing issues: Certain states may require providers who practice telemedicine across state lines have a valid license in the state where the patient is located.
Coverage and cost
There are a variety of payment models to fund telemedicine services. For example, some health systems offer telemedicine consultations as part of their regular care services, and payers charge patients based on insurance plans or government reimbursement schedules. In other cases, a patient's employer offers virtual care options as part of health insurance coverage premiums. Some people may opt to independently use a telemedicine vendor for a flat fee.
Currently, the Centers for Medicare & Medicaid Services is reviewing its proposal to expand telemedicine access and reimbursement in the federal Physician Fee Schedule, including by:
- Paying clinicians for virtual check-ins conducted through communications technology;
- Paying clinicians for evaluation of patient-submitted photos; and
- Expanding Medicare-covered telehealth services to include prolonged preventive services.
United States telemedicine laws
Although the Patient Protection and Affordable Care Act of 2010 governs telemedicine in certain situations under Medicare, telemedicine regulation for the most part falls to the states. As of spring 2018, 49 states and Washington, D.C., provide reimbursement through Medicaid for some version of live video care, according to the Center for Connected Health Policy, a group that promotes telemedicine.
While laws about prescriptions issued through telemedicine consultations are stringent in many states, the general trend is that more states will allow these types of online prescriptions. A sticking point is that prescriptions require the establishment of a doctor-patient relationship and until recently, some states did not qualify virtual visits as a legitimate relationship.
Advances in telemedicine technology
As the potential -- if not the actual success, yet -- of AI grows in healthcare, telemedicine stands to benefit from it. It's not hard to imagine telemedicine chatbots being the initial party that a patient discusses symptoms with during a smartphone video call, and based on AI deductions of the situation, recommendations could follow or an actual physician could join the discussion.
Tied into that theme is how smart speakers may someday play a role in telemedicine, with a consumer at home saying to the speaker, “I need to talk to a doctor about my sore throat right now.” The speaker's virtual assistant software would then search for telemedicine services.
Telemedicine vs. telehealth
Telemedicine used to be considered a subset of telehealth, but the two terms are now used as synonyms.
In the early days of the internet, the label telehealth included nonclinical services such as continuing medical education, provider training and administrative meetings. In contrast, telemedicine originally pertained exclusively to the use of electronic communications to provide clinical services without requiring a patient to come in to a doctor's office or hospital.
In the United States, the Federal Communications Commission sometimes uses the term eCare as an umbrella label any electronic exchange of information that aids in the practice of advanced analytics and medicine.
History of telemedicine
The development of modern telemedicine began with the invention of the telecommunications infrastructure, including the telephone and telegraph. Early on, telemedicine technology was adopted for use in military situations during the Civil War, such as ordering medical supplies or medical consultations. Casualty and injury lists were also delivered via telegraph.
The first example of an electronic medical record transfer occurred in 1948 in Pennsylvania, when radiology images were sent 24 miles between two townships via telephone line. A few years later, Canadian radiologists built on that early application of telemedicine technology and created a teleradiology system for use in and around Montreal. In 1959, clinicians at the University of Nebraska transmitted neurological examinations across campus to medical students using two-way interactive television.
In the early days of telemedicine, health professionals used the burgeoning technology as a way to reach patients living in rural areas. However, the technology quickly expanded into urban areas, especially those that suffered from healthcare shortages.





